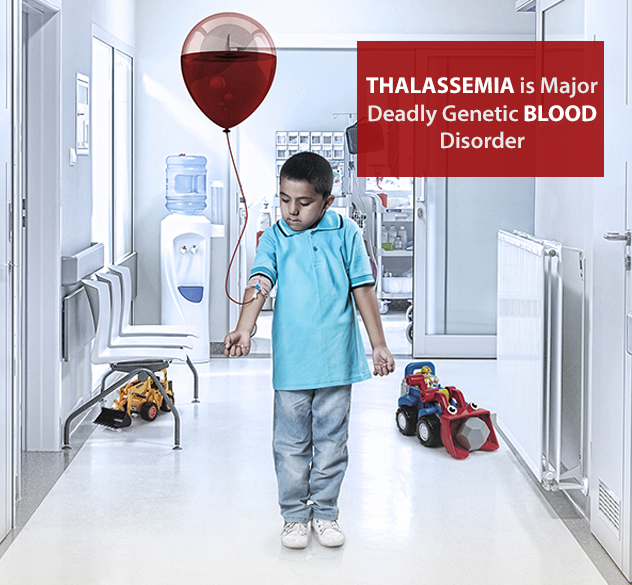
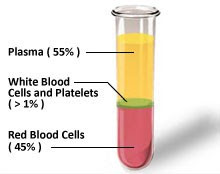
Thalassemia is an inherited blood disorder in which the body makes an abnormal form of hemoglobin. Hemoglobin is the protein molecule in red blood cells that carries oxygen. The disorder results in excessive destruction of red blood cells, which leads to anemia. Anemia is a condition in which your body doesn’t have enough normal, healthy red blood cells.
What Are the Signs and Symptoms of Thalassemias?
- A pale and listless appearance.
- Poor appetite.
- Dark urine (a sign that red blood cells are breaking down)
- Slowed growth and delayed puberty.
- Jaundice (a yellowish color of the skin or whites of the eyes)
- An enlarged spleen, liver, or heart.
 Is thalassemia blood cancer?
Is thalassemia blood cancer?
Thalassemias are inherited blood disorders that cause the body to make fewer healthy red blood cells and less hemoglobin than normal. Mild or severe anemia can also be present in people with thalassemias. The two major types of thalassemia are alpha and beta, named after defects in the hemoglobin protein chains.
What is the disease thalassemia?
Thalassemia is an inherited blood disorder in which the body makes an abnormal form of hemoglobin. Hemoglobin is the protein molecule in red blood cells that carries oxygen. The disorder results in excessive destruction of red blood cells, which leads to anemia.
What is beta thalassemia major?
Usually, they are mildly anemic and their red blood cells are smaller than normal. Beta thalassemia major (Cooley's anemia) happens when both of the beta globin genes are mutated (changed) and the mutations are severe. This is the most severe form of beta thalassemia.
What is thalassemia major disease?
Thalassemia Major. Thalassemia major occurs when a child inherits two mutated genes, one from each parent. Children born with thalassemia major usually develop the symptoms of severe anemia within the first year of life. They lack the ability to produce normal, adult hemoglobin and experience chronic fatigue.
Is there a cure for beta thalassemia?
People with severe thalassemia depend on blood transfusions to give them working red blood cells. A type of bone marrow transplant has been used to try to cure thalassemia, but it's hard to find compatible donors. And even if a donor can be found, there's still a risk that the patient's body will reject the transplant.
What is the thalassemia trait?
Thalassemia is an inherited blood disorder in which the body makes an abnormal form of hemoglobin. Hemoglobin is the protein molecule in red blood cells that carries oxygen. The disorder results in excessive destruction of red blood cells, which leads to anemia.
Can you give blood if you have thalassemia minor?
Yes it is possible for carrier to donate blood if their hemoglobin (iron) level meets the international criteria for donation. Yes it is ok for carriers to donate stem cells, such as those in bone marrow, for his/her diseased sibling. The problem is that carriers could have thalassemia major children.
Is thalassemia more common in males or females?
If both genes are affected, the result is moderate to severe anemia. The severe form of beta thalassemia is known as thalassemia major or Cooley's anemia. Thalassemias affect males and females. The disorders occur most often among people of Italian, Greek, Middle Eastern, Southern Asian, and African descent.